Older adults prefer living independently at home, in their familiar environment, over a longer period of time (Vermeulen, 2006). Facilitating aging in place helps increasing older adults’ quality of life. It enables actively participating in the community and maintaining social networks, increases personal security, and limits the negative effect of relocation, such as confusion, alienation and developing speeding up mental and physical decline. Illustratively, aging in place can contribute to preservation of cognition, decrease in depression, and prevention of incontinence (e.g., Bassuk, et al., 1999; Berg-Warman, 2006; Marek et al., 2005). Maybe most importantly, aging in place offers the possibility to live in an environment which helps older adults to relive old memories dear to them.
In addition, aging in place can contribute to levelling the imbalance in care supply and demand due to the population’s aging. The global population is ageing, i.e., the median age rises, and the number of older adults who are requiring more health care increases1. Illustratively, in the Netherlands, it is estimated that in 2030, over 4 million people, almost a fourth of the population, will be over 65 years old (Blokstra, 2007). As a result, the number of people with chronic conditions is unceasingly rising. Due to aging, people become more prone to chronic diseases, such as diabetes, heart failure and dementia, often suffer from multimorbidity (i.e., multiple, correlated diseases), over an extended period of time. Also, due to aging, there will be a decrease in the number of potential care professionals, which adds to their increasing workload (Bakker et al., 2005). Furthermore, the shortage in the medical workforce will lead to higher care prices and an increase in the economic burden for patients, insurance companies, government and, thus, for society (Druss et al., 2001). The possible impact of this demographic development raises serious concerns and there is urgency in reducing the gap between demand and supply in health care.
An important requirement for aging in place is the ability for people to perform self-care. Self-care is undertaken by individuals, together with families, and communities with the intention of preventing disease, limiting illness, and restoring health (Leventhal et al., 2004).
Examples of self-care activities are maintaining a healthy diet, performing physical activities, using medical instruments, such as glucose and blood pressure meters, setting personal goals and increasing health literacy. Other terms used for increase and maintenance of health are disease self-regulation and self-management, but for this chapter we have chosen the term self-care for its clarity and conciseness.
As illustrated in the following scenario, an older adults’ current living environment does not always facilitate aging in place. Mrs. Brown is an older woman (76) and lives alone and independently at home. Her husband has passed away 5 years before. Mrs. Brown suffers from diabetes type II and recently has developed a light dementia. She prefers to continue living at home to maintain an active and socially participative life. One night, Mrs. Brown did not sleep well. She woke up a couple of times to go to the bathroom and the last time she gets shaky and confused on her way back to bed, possibly due to a hyperglycaemic attack. She panics, trips and falls to the floor. She is not able to send an alarm, because she cannot find the emergency button, nor to find her way back to bed. Her daughter finds her only next morning in a hurt and highly distressed state. As illustrated in this scenario, aging in place poses a trade-off. On the one hand, aging in place contributes to quality of life aspects, i.e., social, mental and physical wellbeing, and, on the other hand, it increases the burden of the older adults to perform self-care and the need for constant monitoring and response in case of acute need for help.
Smart Homes provide a possibility to address this trade-off and support aging in place (Blanson Henkemans et al., 2007). As defined by Demiris and Hensel (2008), “a ‘smart home’ is a residence wired with technology features that monitor the well-being and activities of their residents to improve overall quality of life, increase independence and prevent emergencies.” They offer a promising and cost-effective way of improving home care for older adults in a non-obtrusive way, which allows greater independence, maintaining good health and preventing social isolation. Smart homes are equipped with sensors, actuators, and/or biomedical monitors. These devices operate in a network connected to a remote centre for data collection and processing (Chan et al., 2009). Accordingly, Smart Homes are becoming increasingly popular and are receiving more and more focus as support environments for healthy, socially participating and self-caring inhabitants (Ackerman, 2009).
When taking into consideration the possibilities of Smart Home environments for aging in place, our research question reads as follows: How can Smart Home environments, with its different support functionalities, contribute to aging in place, with the focus on self-care and support of acute health problems? To answer this question, we elaborate on the importance of self-care for aging in place and its implications for support requirements. Subsequently, we will make an inventory of Smart Home functionalities and describe their main characteristics in relation to supporting aging in place. Finally, we will discuss how Smart Homes facilitate aging in place. This chapter concludes with a discussion on how self-care activities and support acute help are supported by applying existing Smart Home functionalities and what the remaining challenges are.
Aging in Place: Self-care for Independent Living
As discussed in the Introduction section, an important aspect in aging in place is the possibility for older adults to perform self-care. People with chronic diseases, such as diabetes, chronic hart failure, and dementia, are faced with psychosocial problems, such as stigmatism; moreover, they need to manage daily living according to their financial and social conditions to be able to live independently at home. Furthermore, patients require sufficient knowledge about their condition and its treatment, performance of condition management activities, and application of the necessary skills to maintain adequate psychosocial functioning (Barlow et al., 2002). Accordingly, self-care aims at educating and increasing the patient’s intrinsic motivation, which in turn can lead to stimulation of maintaining a healthy lifestyle and adhering to medical treatment (Maes & Karoly, 2005). For this, patients need to be provided with relevant medical information and support for developing self-care skills, i.e., problem solving, decision making, resource utilization, forming of a patient-caregiver partnership, and taking action (Lorig & Holman, 2003).
A prerequisite for self-care is the empowerment of patients. Patients should be able to perform self-care activities themselves, but also need to be facilitated by their informal and formal caregivers, such as peer and home care, specialist, and nurse practitioner. Caregivers should empower patients to take their care and health more in their own hand. Whether self-care means taking medication, making life-style changes or undertaking preventive actions, patients must be guided to make their own day-to-day decisions (Newman et al., 2004). This implies allocating responsibility to the patient (Alsop & Heinsohn, 2005), providing education about the illness and treatment options, finding out practical information on healthcare services, and understanding the medical jargon (Barlow et al., 2002). Accordingly, patients and caregivers operate more on the same level, which increase the capabilities of the patient and independence long term.
Based on these theories of self-care and patient empowerment, we define four aspects of self-care, which are the following (Blanson Henkemans et al., 2010): 1. Gaining a good insight in their own health condition;
2. Retrieving personal information to support choices of self-care activities; 3. Fitting self-care activities in daily life and developing self-care habits;
4. Involving the environment to support self-care.
In addition, it is essential for people to maintain a healthy lifestyle, but equally to maintain a good quality of life, i.e., enjoy their social and professional life, have room for personal interests (e.g., hobbies), and maintain a good psychological well being. We will now elaborate further on these four aspects.
First, patients need to gain insight in their own condition. For example, patients with diabetes, such as Mrs Brown in our scenario, are confronted with a great variety of data about their condition. Nutrition, physical activity, monitoring results, and medication are all details related to someone’s health condition. Moreover, it is important for the patient to keep track of the medical condition, current health and the prognosis (Halme et al., 2005). More specifically, keeping track of their diet, physical activities, medication prescription, intake and actual working, and arranging the entries and sharing them with relevant actors, such as family and caregivers, help people to better understand their current conditions and possibly to foresee possible upcoming complications.
Second, people need to acquire information about their condition, such as its background, consequences and treatment possibilities, and develop health literacy (Murray et al., 2004b). Based on this information and insights in their own condition, patients can evaluate and choose between different personally preferred self-care options (e.g., change of life style, medication intake, surgical operation, or non-treatment). The choice is based on the consequence of their choice on important life domains, such as work, family, social life and hobbies. Information can help structure the possibilities and help making the most fitted choice (Thun et al., 2008; Woloshin et al., 2000). Specifically, older adults who are in receipt of information geared to their personal characteristics (e.g., medical history, phase of disease, treatment, and norms and values), will translate their condition insights into selfcare activities better. They can weigh off the consequences of certain self-care choices on their health against their constraints for important life domains, such as participating in (voluntarily) work and social activities and hobbies.
Third, the selected self-care activities need to be developed into habits, combined with daily activities. Here, translating a treatment to personal goals and setting plans to achieve those goals are essential (Lorig et al., 2006). People want to adhere to their treatment, e.g., treat their diabetes, which requires the motivation to perform certain activities, such as exercising on a daily basis. This implies that they have to internalize their treatment (Deci & Ryan, 2002), i.e., determine their preferences and intentions, problem solve probable pitfalls, and then make their activities specific, measurable, acceptable, realistic and time bound (SMART) (O’Neill et al., 2006). Illustratively, Mrs Brown, who decides to perform exercise regularly can plan an half hour mall walk, on every Monday, Wednesday and Saturday, which are the days mall walks occur and her daughter or neighbour is available to pick her up because she goes shopping on those days. After three months she checks if she indeed participated, on average, in two walks a week and what effect it had on her HbA1c (i.e., average glucose level over a period of three months) and general physical mobility. The latter implies monitoring and providing feedback which, in line with the motivational interviewing approach, applies an empathetic perspective and focuses on increasing selfefficacy, stimulating self-reflection and offering guidelines for independently overcoming challenges, which can contribute to realizing these self-care habits (Rollink et al., 2008).
In the discussion on self-care activities, we already mentioned repeatedly the importance of the environment. Involving family members and neighbours is good example, as is joining clubs in the community that can give social and possibly, health support. Also peer, home and specialist care need to be involved. To realize this, the older adults need to organize the support of partners, family members, neighbours, community centres and informal and formal care. For this organization, acquiring information about possible support is essential. Moreover, it will contribute most to aging in place when the support is provided integrally, i.e., each actor plays a role, collaboratively, in the care of the patient and the support of selfcare (Molema, 2009).
In relation to patient empowerment, the older adult in a home situation is better positioned to be aging in place, when three main requirements are met, which are:
– Access to information about illnesses and diseases, available health care services and care options and to tools such ICT-based applications or medical devices;
– Skills to carry out self-care activities (such as problem solving, understanding, decision making);
– Motivation to achieve one’s own goals. Information and services tailored to the person’s own health situation (personalized and contextualized) are also intertwined to these requirements.
These requirements of empowerment are facilitated via a number of patient-centred mechanisms, which enable communication, provide education and raise the level of health literacy, provide information, enable and support self-care practices, provide decision-aids, support contact with fellow patients, and facilitating integrated care (Monteagudo & Moreno 2007; Aujoulat et al., 2008).
Finally, older adults are faced with dynamic age related factors, such as cognitive, sensory, perception, and movement skills, and with the side effect of their health condition. This poses additional challenges in living independently, with the use of technical support offered (Fisk et al., 2009), and as a result may constrain the possibilities of aging in place in Smart Homes. Table 1 presents a description and examples of the different age related factors and gives possible constraints for aging in place support. As an illustration of the effect of age and condition related characteristic on aging in place, older adults with diabetes type II can experience difficulties remembering their medication, which possibly leads to an acute hyperglycaemic attack. When offering technical support in the form of visual and additive support (e.g., computer display providing textual instructions about what to do, accompanied with speech), both dizziness, shakiness and confusion, as an effect of the attack, and cognitive overload, due to multitude of multi-perceptive modalities, can negatively affect the usability of the support. Consequently, when supporting self-care activities and offering acute help, it is important to take into consideration the personal requirements of the older adults to realize success with the offered supporting mechanisms, such as alarms, complex notifications with large amounts and layered information and interfaces that require detailed manipulations.
In summary, to support aging in place, it is important to facilitate self-care and promote patient empowerment. Patients need to be able to gain insight in their condition, acquire information related to their condition and their personal preferences, translate their treatment to personal life style goals, and involve the environment in their self-care. Patient empowerment, which focuses on making accessible of personal information about health and care, training skills to cope with the illness and motivating to set and achieve own goals, plays an important role in facilitating self-care. Finally, age related factors, i.e., cognitive, sensory, perceptive and motor skills, impact how well support is geared to personal requirements and need to be taken into consideration when offering support for aging in place, relating to communication, education information, decision-aids, fellow patients forums, and integrated care.
Smart Home Initiatives
Demiris & Hensel (2008) gave an elaborate systematic review of health related Smart Home projects. Their international inventory (i.e., United States, Europe and Asia) covered 21 smart home initiatives, including the Aware Home Research Initiative at the Georgia Institute of Technology; Place Lab, Massachusetts Institute of Technology, ENABLE project, which is a joined initiative from UK, Ireland, Finland, Lithuania and Norway, Philips Care Lab, Eindhoven, the Netherlands; PROSAFE in Toulouse, France; Welfare Techno-House project, Japan. Across these different initiatives, the authors identified the following functionalities present in Smart Homes:
1. Physiological monitoring of physiological measurements (e.g., pulse, respiration, temperature, and blood pressure, as well as blood sugar level);
2. Functional monitoring of functional measurements (e.g., motion, meal intake, and other activities-of-daily-living, whereby abnormal or critical situations (e.g., falls) are detected;
3. Safety monitoring and assistance of environmental hazards (e.g., fire or gas leak). Assistance includes automatic turning on and off bathroom lights when getting out of bed and facilitating safety by reducing trips and falls;
4. Security monitoring and assistance of domestic threats (e.g., intruders). Assistance includes notification of external relevant actors;
5. Social interaction monitoring and assistance of social interactions (e.g., phone calls, visitors, and participation in activities). Assistance includes technologies that facilitate social interaction (e.g., video-based components that support video mediated communication with friends and loved ones and virtual participation in group activities);
6. Cognitive and sensory assistance of automated or self-initiated reminders and other cognitive aids for users with identified memory deficits (e.g., medication reminder and management tools, lost key locators). Aids include task instruction technologies (e.g., verbal instructions in using an appliance) and aids for sensory deficits (e.g., sight, hearing, and touch).
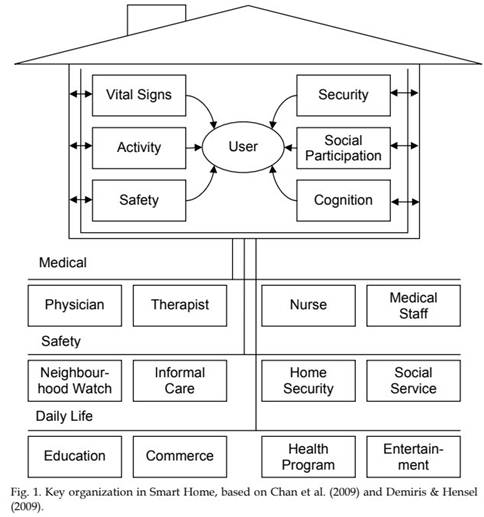
By offering these functionalities, integrated as illustrated in Figure 1, Smart Homes pose interesting benefits. Chan and colleagues (2009) point out the following possibilities of Smart Homes. First, through the different monitoring possibilities, they enable measurements of vital signs and behavioural patterns, which can be translated into accurate predictors of health risks and combined with alarm-triggering systems to initiate appropriate medical action. Second, the monitored data can support transmural care (Celler et al., 2003). That is to say, they facilitate an infrastructure for coordinating multidisciplinary care outside the hospital (scheduling visits with health staff and community health workers, automating collection of clinical findings and test results) and providing means for nursing services in the home (Finch et al., 2008). Third, through cognitive, sensory, and socially participation monitoring and assistance, Smart Homes can stimulate patient-centred care (Paré et al., 2007). The offered functionalities enable a patient-centred management approach that provides accurate and reliable data, empowers patients, influences their attitudes and behaviours, and potentially improves their medical condition. By providing accurate and up-to-date information, to help take better decision, patients become more responsible, informed, expert, and educated self-managers. Fourth, Smart Homes offer economic benefits. The use of functionalities in the form of, for example, personal health records (PHR), e-prescribing, decision support systems, electronic management of chronic illness, can contribute to increasing care efficiency. This is due to time and cost reduction, reducing care need through prevention of illness deterioration, and supervising and early establishing medical errors (Anderson, 2007). Finally, Smart Home Labs, such as the Georgia Tech Aware Home, offer a testing ground for generic environmental constructs and their measurement, as well as a unique setting from which new understandings of personenvironment fit can emerge. Essentially, Smart Homes offer a domestic environment for natural use of technology in a controlled and observational environment (Blanson Henkemans et al., 2007).
Another interesting development in Smart Homes is the use of robotics. In the domain of health care, robotics can be deployed for five objectives (Butter et al., 2008):
– Assisting in preventive therapies and diagnostics, through robotized analysis of motion and coordination, intelligent fitness systems, tele-diagnostic and monitoring robotics systems, and smart medical capsules;
– Facilitating people with disabilities and chronic conditions to continuously perform their daily activities, through robotized systems supporting manipulation and mobility, and intelligent prosthetics;
– Assisting professional care giving, through robotized logistical aids for nurses, patient monitoring systems, physical tasks in care provision, and paramedic tasks;
– Rehabilitating patients, through robot-assisted motor-coordination, physical training and mental cognitive and social therapies;
– Supporting surgery, through robot-assisted precision, minimal invasive and remote surgery, and medical micro- and nanobots.
Due to this wide range of application possibilities, robotics can contribute to reducing labour costs, increasing independence social independent, quality of care and, the performance of activities otherwise not executable for humans, such as lifting heavy weights.
In addition, due to their physical appearance, they are able to offer assistance in a social intelligent manner (Looije et al., 2009). A social intelligent robot that offers three support roles, i.e., educator, motivator and buddy, can respectively inform patients with diabetes about their illness, guide self-care goal-setting, and offer empathetic feedback to help attaining them. Moreover, by assessing personal characteristics, recalling previous interactions, and having a social dialogue (with gaze, facial expression, and vocal intonations), the robot could develop an inspiring relationship with the patients (Blanson Henkemans et al., 2009).
An aspect we need to address, when stating the advantages of Smart Homes is the deficiency in empirical research. When we look at the reviews of Demiris and Hensel (2008) and Martin et al. (2008), a number of shortcomings are found in current research. Most of the studies are pilot or short-term projects, consisting of nonrandomized trials without control groups, which often show methodological weaknesses (e.g., in samples size, context, and study design), limiting the generalization of the findings. Also, the few randomized controlled trials that are conducted refrain from comparing Smart Home interventions with conventional health care practices. Accordingly, although the current literature depicts great potential of Smart Homes for aging in place, it is currently difficult to accurately point out their clinical and economical benefits.
Smart Homes for Aging in Place: Application and Challenges
In the future, Smart Homes can add to performing self-care and, accordingly, to aging in place. An integrated system of different functionalities, which monitor and assist psychological and functional functioning, safety, security, social interactions and providing cognitive and sensory assistance, will be offered through various devices, such as Information and Communication Technology (ICT) and robotics (e.g., assistive device, robotic-assistant, companion robot, autonomous wheelchair, and stair lift). These devices are capable of providing support for making decisions and diagnoses, improve inhabitants’ access to health care services and optimizing resource utilization, control of home appliances, such as heating, air-conditioning, windows, and stoves.
In addition, when we look at transmural care support for aging in place, Smart Homes are connected to hospital, which increasingly become a central health information centre. Accordingly, these centres direct activities in the Smart Homes, supported by technology on location, which decreases the requirement for people to be hospitalized for their condition. For example, hospital-based health professionals can initiate consults online, i.e., eConsult, and make virtual visits to the patient, and specialized care tasks can be reallocated to mobile health professionals with technical support on location.
Application of Smart Homes for Aging in Place
As illustrated in Figure 2, following are a number of Smart Home applications for aging in place. People with dementia can be navigated by a pet robot to find their bathroom during the night and return safely to bed. Moreover, the bathroom contains a number of sensors that can monitor vital functionalities, which enables diagnosis and possible early detection of physical complications. The collected data is stored in a PHR, managed by the inhabitants and (remotely) accessible for the people they feel appropriate. Movement sensors are set throughout the house, which detect movement and can infer unusual patterns, or lack of movement. For example, when a person falls and stays immobile on the floor, a notification can be sent to neighbours, family or relevant caregivers.
eConsults are made possible through personal computers and on large screens throughout the house with interface specifications geared to aging related characteristics (e.g., big font, recognizable colours, singular perceptive modalities, and information provided in small doses). People in Smart Homes can virtually consult with caregivers, which includes elaborate educational modules that provided information related to the treatment and topics discussed. Because the service is accessible when relevant and convenient for the patient, it can increase personalized access to information and training of skills to translate prescribed treatment to self-care activities. Virtual meetings can also be put into practice to communicate with family, people in the community, peers, and even a computer coach, i.e., an eCoach, for empathetic motivating and educational support and also entertainment, which can increase the quality of life. The eCoach can be presented on the computer and as mobile social intelligent robot.
In addition to their social role, robots can also help with daily household activities, which become challenging for the inhabitants, enabling them to stay longer independently in their home. Exemplary activities are cleaning, filling and emptying the dish washer, supporting mobility in the house (e.g., walking the stairs) and outside the house (e.g., gardening, doing groceries, and meeting people in the neighbourhood). Moreover, they can support home care with their activities, such as lifting people out of bed.

Fig. 2. Smart Home Environment facilitating aging in place.
Challenges for Smart Homes for Aging in Place
Despite the vast proposed benefits Smart Homes have to offer, there are still a number of challenges in relation to supporting self-care activities and, thus, aging in place. The first challenge is the standardization of the technology in the environment. Professionals outside a networking system are faced with lack of ability to exchange clinical data with laboratories and hospitals. Also, because the industry that delivers the functionalities for Smart Homes tends to be dominated by suppliers the common approach is technology-push, rather than a demand-pull approach, which causes lack of user centred design (UCD) and, thus of user friendly applications.
As we saw in Table 1, gearing to users’ needs is specifically important when supporting older adults with aging in place, since they are faced with dynamic sensory, perceptive, cognitive and movement skills, and standard support technology may greatly neglect their personal requirements (Fisk et al., 2009). Lack of usability leads to decline in self-efficacy and to mistrust in relation to the technology, which in turn elicits breached privacy feelings.
Introducing technology in the house could trigger several issues: accidental disclosure of individuals’ data, contacting the wrong people, and incorrect use of data (Croll & Croll, 2007). As a result, in case of mistrust, the inhabitants of Smart Homes may decide to withhold information, disclose obscured data to health care providers, or avoid using the health care support system altogether, which goes at the cost of the effectiveness of the Smart Homes’ functionalities. Lack of usability may also lead to the conception that technology will replace personal interaction with their health care providers and they may worry about a technology affecting their lifestyle, financial status, emotional and psychological wellbeing of family members (Bauer, 2001).
In summary, UCD needs to be a constant factor in and throughout the development of technology and implementation in Smart Homes (Vredenburg et al., 2002). Users, including inhabitants, people in their environment, caregivers and stakeholders, such as hospitals, insurance companies, industry, and policy makers, are involved early in setting up of design specification, designing and evaluating prototypes, and in the implementation process (Blanson Henkemans et al., Submitted). The latter implies that the goal and background of the technology is explained in a way understandable for the user, whereby special attention goes out to ethical issues (Bauer, 2001), and its introduction is elaborately guided.
Discussion
People prefer living longer and independently at home, but aging in place poses a thorny trade-off. On the one hand, it contributes to older adults maintaining a mental, physical and social wellbeing and adding to their quality of life. On the other hand, because older adults are often faced with one or multiple chronic conditions, their wish to age in place compels them to perform complex self-care activities, preventing disease, limiting illness, and restoring health. Moreover, there is a need for constant monitoring in case of acute need for help, i.e., when health threatening situations occur. Smart homes, i.e., residences containing technology that monitor the well-being and activities of their residents, become increasingly popular and receive more focus as support environments for healthy, socially participating and self-caring inhabitants (Demiris & Hensel, 2008; Ackerman, 2009). Accordingly, in this chapter we studied how Smart Home environments, with its different support functionalities, can contribute to aging in place, with the focus on self-care and support of acute problems with their wellbeing.
In line with the research on self-care (e.g., Barlow et al., 2002; Leventhal et al., 2004; Lorig et al., 2003; Maes & Karoly, 2005), we elaborated on the importance of self-care for aging in place and its implications for support requirements. Based on these theories, we defined four main self-care activities for older adults aging at home, which are: gaining a good insight in the personal health condition, retrieving personal information to support choices in self-care activities; fitting self-care activities into daily life and developing healthy habits; involving the environment to support self-care. To increase the chances for people to actually continuously perform these self-care activities, it is essential to facilitate combining a healthy lifestyle with a good quality of life, i.e., enjoy their social and professional life, have room for personal interests (e.g., hobbies), and maintain a good psychological well being (Blanson Henkemans et al., 2010). Moreover, both health condition, e.g., shakiness and aggravation, and age related factors, i.e., cognitive, sensory, perceptive and motor skills, impact how well Smart Home functionalities are geared to personal requirements and need to be taken into consideration when offering support for aging in place.
When looking at the literature (e.g., Demiris & Hensel, 2008; Martin et al., 2007; Chan et al., 2009), Smart Homes offer the possibility to monitor and assist physiological and functional activities, safety, security, and social activities. Also, they offer cognitive and sensory assistance. These functionalities are offered by integrated technology, such as computers, databases, sensors, video cameras, interfaces (e.g., monitors) implemented ubiquitously in and around the house and in connection with remote actors, such as family, caregivers and other supervising units. In addition, robots active in the Smart Home environment offer the possibility of mobile guidance and physical support (Butter et al., 2009).
An important benefit of Smart Homes for aging in place is online monitoring of the inhabitants’ vital, movement and general wellbeing data and their transfer to supporting actors, such as family, peer and home care, and specialists. Also, with technology on location, caregivers become less reliant on the hospital or clinic, making them more mobile, enabling multidisciplinary care in the home (Finch et al., 2003), and facilitating patientcentred care. Illustratively, in Smart Homes, care can be offered virtually (e.g., eConsult), remotely coordinated (e.g., nursing service remotely guided by specialists) and directly (e.g., professional linked to the hospital, which functions as a central health information centre). The appropriate type of care can be selected depending on the health condition and preferences of the patient. Finally, with the use of robotics, daily activities that become challenging for older adults can be supported by robots. For example, emptying the dish washer can be fully allocated to the robot assistant, doing gardening can be supported by an exoskeleton robot that facilitates continuous mobility, and going to the bathroom at night can be guided by a robotic pet dog, with directing spotlights and distinct noises.
Challenges that need to be overcome lay in the realm of experienced usability of the Smart Home technology by the inhabitants, their environment and the caregivers. When they are insufficiently involved in the development and implementation process, caused by a technology-push approach (Barlow et al., 2006), users may mistrust the technology in their house and question the ethics, considering the strong focus on monitoring. This may lead to obscured data and to ineffective Smart Home support, accordingly. Another result is that people feel that technology is posed upon them and may replace personal interaction with their social environment and health care providers. The technology is foremost a facilitating tool to enable aging in place by complementing human care and not by replacing it. Only when it is apparent to the users, including the caregivers, that the technology is there to meet with this facilitating function and fit with their daily life objectives, e.g., participating in social activities, maintaining hobbies, and receiving and providing personal care, will Smart Homes be fully adapted.
Strikingly, although indicated as one of the possible benefits by Paré et al. (2007), the established Smart Home functionalities offer little concrete support to elicit intrinsically motivated self-care activities. The main focus lies in monitoring and offering accurate and up-to-date information to help older adults to make better decisions and become more informed. This may indeed help managing medical and wellbeing data, receiving personalized information and involving actors the environment with self-care activities. However, besides the use of social intelligent robots as motivating partners (Looije et al., 2009), little attention goes out to translating treatment to personal self-care goals, to planning, attaining, and maintaining them, and to iterative provision of empathetic, selfreflective and empowering feedback. As a result, with the currently developed Smart Home functionalities, people may understand their condition and decide what self-care activities to perform short term (e.g., maintaining healthy diet, exercising regular, and taking medication) and may be met in their acute care needs, but will experience challenges to actually put it to practice long term and develop healthy habits required to age in place (Deci & Ryan, 2002).
The theory on self-care, as described in this chapter, provides useful guidelines to develop the functionality for developing healthy habits, but assessing how practically developing and implementing it asks for an extension in user-centred and empirical research in relation to the effect of Smart Homes on quality of life (e.g., functioning, emotional well-being, social involvement, and satisfaction), clinical outcomes, and financial benefits (Vredeburg et al., 2005; Cutler, 2007; Gitlin, 2003). Interestingly, Smart Homes, with their monitoring facilities, offer great testing ground possibilities. Of course, as with monitoring in non-experimental Smart Homes, special attention needs to go out to the (medical) ethical issues, such as the guarantee of voluntary participation and a good balance between participants’ risks and social and scientific benefits.
When augmenting current monitoring and assisting functionalities with support of long term self-care, in regards to setting, attaining and maintaining personal self-care goals, Smart Homes offer great potential for aging in place. As illustrated in the following scenario, this can help increasing quality of life, by enabling actively participating in the community and maintaining social networks, increases personal security, and limits the negative effect of relocation (e.g., Berg-Warman, 2006; Marek et al., 2005). Moreover it can contribute to levelling the forecasted imbalance in health care demand and supply, as described in the following scenario. Mrs. Brown experiences some problems with her glucose level and needs to go to the bathroom multiple times throughout the night. The sensors in her Smart Home detect her movements and instruct the pet robot to physically guide her to and from the bathroom. Based on the detection of unbalanced movements and vital signs (e.g., excessive perspiration), her eCoach suspects a health issue (e.g., glucose level too high) and instructs her service robot to measure her glucose levels and administrate insulin accordingly. The dosage and intervention time are registered in her PHR. Also, both her daughter and the personal diabetes nurse are notified of the occurrence, including the severity, and the latter comes by to check with Mrs. Brown the next morning. She compliments her on how well it goes with her living independently. Later that day, her daughter visits and together they go for a healthy walk to the botanical gardens.