Traditional smart home (SH) technology combined with new monitoring technologies designed to prevent falls and detect health status changes is the current direction for SH development. The combination of conventional SH technology with healthcare technology is likely to be an effective approach to preventing nursing home placement for frail older adults.
Barriers to adopting or implementing monitoring technology include concerns about privacy and reluctance of older adults to accept the technology. Acceptance of the monitoring technology depends not only on the older persons’ health and functional status but also upon the perception of need and personal goals. Since great variability of health and disability conditions exists among community-dwelling older adults, their purposes of using SH with healthcare technologies may also be diverse depending on their levels of physical and cognitive functions and severity of illnesses. Older adults and their informal caregivers are likely to insist on choice of technologies suitable for their goals. Health care providers need to be familiar with the available technology.
Home-based technologies allow older persons to adapt to changing physical and cognitive function and preserve living in a familiar environment within an established social network. Home-based technologies may be most effective, if they also promote healthy behaviour and lifestyles for continued community living.
Focusing on the situation in the United States, this chapter includes: (1) a description of societal needs for the technology, (2) a summary of current SH status, (3) a review of older adults’ perceptions of SH, healthcare technologies and their effectiveness, (4) caregivers’ perspectives of the technology, and (5) defining the role of SH with health care technologies in the Model toward Optimal Management for Independent through Technological Adoption (Tomita et al., 2009). The model expands on behavioural medicine to promote healthy behaviours in community-dwelling older adults.
Societal needs for smart home and healthcare technologies in the United States
The United States is experiencing a rapid increase in its aged population. An aging population is associated with an increase in the incidence and prevalence of chronic diseases and an increase in health care expenditure (Administration on Aging, 2008). In 2000, the total Medicare expenditure was $239.5 billion; 10 years later, in 2010, expenditures are expected to rise to $519 billion (Foster, 2008). As 77 million baby boomers (born in 19461964) begin to reach age 65 in 2011, it is forecasted that Medicare expenditures will explode. Aging in place has been proposed as one method to reduce cost and maintain quality of life for the aging population. The concept is to support older adults in the environment of their choice in lieu of institutionalisation or nursing home placement. To make this supportive healthcare possible, medical/health monitoring devices and e-health technology have been developed. Use of these technologies in a home setting is still at its dawn, but this method appears to be one of the most promising approaches to facilitate independent living in community-dwelling older adults when the use of the Internet is rapidly increasing. When a health monitoring system is imbedded in a smart home, older people can live in their home while receiving medical support. This idea has been addressed by Stefanov, Bien, and Bang (2004) of the health monitoring subsystem as an important component of SH.
Although SH with health monitoring system appears to be among the most promising methods to facilitate continued community dwelling among older adults, there are many unanswered questions. A world-wide study of longevity tells us that “de-convenience” is important to increase the amount of daily activities for a healthy and longer life (Pinkus, 2009). A healthy life requires physical activity and human connections to facilitate a healthy lifestyle. The convenience of remote control for televisions may compromise a healthy lifestyle. SH technology faces the challenge of convenience and the technology may reduce rather than promote human contact. Reliance on SH technology needs to balance convenience with the need to foster healthy behaviour and social interaction.
Current smart home with healthcare technologies status in the United States
In this section, a current status of SH with healthcare technologies for community-dwelling older adults in the United States is summarized in several categories: laboratory setting, prototype of SM, SH in use, and retrofitted SH. SH technologies in nursing homes are excluded in the summary.
Laboratory setting
SH with healthcare technology for older adults can be found most commonly in a laboratory setting at a university which utilizes an infrastructure equipped with sensors, panels, cameras, etc. The purpose is usually to research older adults’ behaviour in a home environment.
The Smart Medical Home at University of Rochester’s Center for Future Health at the University of Rochester, NY, is one example. The five-room house has infrared sensors, computers, biosensors, and video cameras. Some of the research involves a medication advisor who can converse with a research subject and advise on medication management and dietary adherence, provide memory assistance, and assist with Smart Bandage. Smart Bandage seeks to decrease the burdens of chronic wound care at home. (Center for Future Health, 2005).
When this smart home is applied in a real setting, the integrated technologies may allow residents to maintain health, detect the onset of disease, and manage disease. Future applications include gait monitoring, and observation of behaviour and sleep, and adherence. The Smart Medical Home was designed for adults of all ages, but it is not meant for actual habitation.
Prototype of smart house
Gator Tech Smart House at the University of Florida-Gainesville’s Mobile and Pervasive Computing Laboratory is a comprehensive laboratory-house created to assist older adults in maximizing independence and maintaining higher quality of life (Helal et al., 2005). The entire house is equipped with (a) smart cameras for motion detection, image processing, and control of other in-home devices, (b) smart blinds that automatically close to block sunlight when the air conditioner is on, (c) ultrasonic location tracking transceivers that are installed on the ceiling corners of each room to detect movement, location, and orientation of the resident, (d) smart floor that uses pressure sensors embedded into each tile to detect falls and reports to emergency services, and (f) smart displays for entertainment media and information residents can follow from room to room. Additional features include a smart mailbox that senses and notifies the arrival of mail, a smart front door that identifies residents, using a radio-frequency identification tag among others, a smart bed that monitors sleeping patterns, a smart mirror that displays important messages or reminders such as when to take medication, and a smart bathroom that includes a toilet paper dispenser, a flush detector, and a water temperature regulating shower. The Gator Tech Smart House is adding healthcare technologies to assist diabetes management (Helal, Schmalz, & Cook, 2009).
Similarly, a SH apartment called CASAS in the Washington State University has seventy motion detectors on doors, a regenerator, a microwave oven, under the sink, a bed, etc. to train a computer to monitor activities of daily living of people who have dementia, and when urgent situations arise, alert caregivers. The sensors and computer hardware were mostly purchased off-the-shelf. But other technologies such as software programming, pattern recognition, and artificial intelligence are being developed (KUOW, 2008).
Both the Gator Home and CASAS have integrated health monitoring software components within a comprehensive monitoring system; this is called the smart home-based health platform. For this, they took an approach to probabilistically identify activities in a SH from sensor data, while the activity is being performed, using a hidden Markov model. Data from the comprehensive monitoring system supported development of a mathematical model to describe sensor patterns for a given activity and for change in activity. The technology monitors diabetic patients’ diet and exercise adherence, in addition to home-activities (Helal, Schmalz, & Cook, 2009). Neither Gator House, nor CASAS is designed for actual habituation.
Research continues with these prototype homes. A two-story single-family house called Aware Home by Georgia Institute of Technology (Atlanta, GA) is a living laboratory house designed primarily to assist an older adult with cognitive impairment. (Do, 2008). For example, there is a capture system on the kitchen countertop. If a person forgets how many cups of flour to put in a mixing bowl, a wall display shows visual snapshots arranged as a series of panels for him/her to touch for review of activities. A similar system can be used to support safe and complete medication adherence (Georgia Institute of Technology, 2009). While most of the technology in Aware Home is for older adults with cognitive deficit, healthcare technology was also developed for diabetes management in individuals without cognitive impairment. Mobile Access to Health Information is used to record readings through verbal descriptions and pictures. It uses a mobile phone to which a glucose meter can be connected via Bluetooth. This captures the impact of recorded activities on blood sugar and is available on password-protected websites. Health technology does not have to be home-bound.
Smart homes in use
Recently, advanced SH technologies have been implemented in actual community settings, apartment complexes, and retirement housing units. A smart home in Vinson Hall Retirement Community in Missouri is dedicated to serving former U.S. military officers and their families. It includes different coloured lighting to help people with vision impairments, a contiguous channelling kitchen where residents can move heavy objects without lifting, and a garbage can that opens with a wave of the hand. In this home, technology is designed to be less obvious and to feel as though it is part of a normal home. For example, grab bars in the bathroom look like upscale towel bars. (Crawford, 2009).
Eskaton, Ltd. created the National Demonstration Home in California with a range of technologies. The combination of SH and healthcare technologies includes a home monitoring system, Internet and teleconferencing abilities, brain fitness activities, and a wellness monitoring station that transmits daily health reports to caregivers. This home utilizes universal design features including a no-step entry, reduced height cabinetry, and an accessible flow to the floor plan. The universal design features cost an additional $4,000 – $8,000 for the 1,600-square-foot floor plan; residents pay an extra $100 to $150 a month to access the technology (Crawford, 2009).
The University of Missouri-Columbia integrated sensor networks into privately owned apartments called TigerPlace II. In the apartments, a health monitoring system detects changes in behaviour and physical activity, including walking and sleeping pattern without compromising privacy. Small sensors over the toilet, shower, and doorways detect residents’ movements. Pneumatic tubes under the mattress and a chair measure weight. The assumption is early identification of older adults’ behaviour changes can prompt healthcare interventions to delay or prevent serious health events. In addition, web-based information is available to healthcare providers (ANI, 2008). This system has been installed in 22 units and currently is in use (Medical New Today, 2009). This system proved effective for at least one resident. The resident’s caregiver and researchers at the University of MissouriColumbia identified patterns in the data that signalled exacerbation of congestive heart failure. Early intervention reduced severity of the episodes.
The most recent development in SH in the United Sates can be found in the McKIZ Aware Community in McKeesport, Pennsylvania. Located in an urban 10-acre, 12-block area. This is the first community-wide comprehensive research project. Although this community is still in a developmental stage, smart homes have been used for actual habitation. In addition, the community will have recreation facilities, retail and service providers on city streets, and public transportation (Wactlar et al., 2009). The purpose of this community is to research individuals with decreases in instrumental activities of daily living (IADL). The infrastructure is designed to monitor activities inside and outside home.
In this community, Blueroof Technologies, a non-profit corporation, has developed the Smart Cottage for older adults. The cottage includes comprehensive home monitoring and Internet access designed for access, energy conservation, safety, convenience, and health maintenance. Eventually the community is planned to have over 100 residents occupying 40 dwellings, of which 60% will be older adults.
All homes in the community will be equipped with high speed Internet access and ZigBee monitoring which will be delivered by wireless transceivers. The transceivers will be integrated into a neighbourhood mesh that will deliver Internet access and energy control, media, and security monitoring to each resident in each home, which will be also connected through one private multifunctional network. Data collected from each home will be stored in a central server for data analyses. The 10 types of technologies used in each home are for: (1) energy management by wireless remote adjustment of thermostat, and automatic cutback on peak at night when unoccupied; (2) appliance (water and stove) and lighting control; (3) video monitoring via a front door camera modulated onto a TV channel; (4) video conferencing used for family communication, medical, and shopping purposes; (5) security for fire, smoke, and carbon monoxide alarms, window and door intrusion, and motion/temperature sensing; (6) health monitoring such as blood pressure, weight, medication management recording, and gross resident activity measures; (7) safety through activity monitors and alert buttons, and fall detectors; (8) wellness including diet, exercise, and preventive medicine; (9) Cyber Nurse allowing patient visits each day via the Internet, video conferencing to see and talk with patients, and recording patients’ activities; and (10) Media Center to interface with the home’s technology including an LCD TV/computer monitor.
Outside these homes, cameras will be installed throughout the community to monitor and record the activity of the community. Since this community level of intervention is a next generation project, only a brief description is made here. The purpose is for older adults with cognitive impairment to be able to participate in IADL such as shopping, crossing a road, and visiting someone by monitoring and supporting their activities. The main contributors of this project include researchers and developers from Carnegie Mellon University, Penn State University, and Blueroof Technologies, Inc.
Smart homes are becoming more inclusive of healthcare technologies and technologies to improve IADL, as well as even basic activities of daily living (BADL), in addition to the original purpose of added convenience. The previous examples of SH are newly built houses or residential complexes. However, the silver tsunami (baby boomers coming to age) will bring increasing demand for SH and healthcare technologies that can be added to existing structures because older adults wish to live in a familiar environment.
Cyber security issues
When a monitoring system is involved in a SH, the concern of security becomes a major issue. Due to the cyber-enabled mode of operation, information and network security are crucial issues for SH with healthcare technology. In addition to traditional physical home security requirements, SH adoption requires to solve novel cyber security vulnerabilities deriving from the network interconnection of different monitoring devices and SH terminals. Busnel (2008) has summarized the security requirements of a SH environment as follows:
Confidentiality: All communication between the SH terminals, monitoring devices and Emergency Response Centre (ERC) should maintain strict confidentiality. Patient’s data available at SH terminals should be accessible to authorized requesters by enforcing standard authentication mechanisms.
Integrity: All the data being exchanged in SH environment should have guaranteed data integrity verification methods. Specially, data communication in SH environment is by and large wireless which is very susceptible to interception as it does not have the shielded protection of wired technology. Any data modified or altered during communication may cause inaccurate decision supplied for treatment planning and delivery.
Availability: The communication between the monitoring devices, SH terminal and ERC should be available on a continuous basis. The network could be proactively monitored for any disruption or anomaly in communication.
Therefore, non-compliance with the aforementioned requirements will leave the information in SH environment vulnerable to different cyber attacks. For instance, one threat to the availability requirement is a Denial of Service (DoS) attack which can lead to severe consequences. Proactive DoS attack mitigation techniques (Lee et al., 2008; Husain & Sridhar, 2009) should be adopted due to the time-critical nature of information exchanged in SH environment. Hash function based message authentication codes (Bellare, Canetti, & Krawczyk, 1996) can be used to maintain data integrity. To maintain data confidentiality, computationally efficient encryption solutions should be considered as most of the devices in SH environment are resource constrained (Oliveira et al., 2007; Sankaran, Husain, & Sridhar, 2009). These solutions, once customized for SH with healthcare technology, can ensure the necessary security required for optimal performance.
Retrofitted smart home and healthcare technology
Although individual cases of existing home retrofitting to smart homes may exist, there are few reports of systematic efforts made to convert to smart homes. Infrastructure wiring essential to SH technology is a major barrier to retrofitting older homes and apartments. For existing structures, among plug-and–play technologies, X10 devices have the longest history and been most extensively utilized.
The University at Buffalo, State University of New York, utilized X10 devices to retrofit 50 homes for older adults with chronic conditions living alone in their own home. X10 is a communications device that allows compatible products to connect to each other using the existing electrical writing in the home. Wireless motion detectors and hand-held remote controls utilize a radio frequency link. The detailed information for the installation and problems encountered for the process and their solutions can be found in the Aging and Technology Research website.
In the beginning, automatic, controlled lighting in each room was one of the most favoured smart home features. At the same time, lighting was the most troublesome feature because it was difficult to re-start after a power failure or when switches were inadvertently turned off. Door and window security, an automatic coffee maker, a security camera connected to lighting and alarm, and a medication reminder were other technologies utilized (Tomita et al., 2007). Its effectiveness has been tested, but this project did not incorporate healthcare technology except for a personal emergency response system. The effectiveness of this system for their caregivers was measured (see the report later in this chapter).
The University at Buffalo also conducted a pilot study for e-health for patients with heart failure (Tomita et al., 2009). In this project, patients used the Internet and daily recorded their vital signs and health behaviours on a website that were monitored by health professionals. Changes in health status alerts were sent to the patient and health care provider. Participants in the intervention group had improved health outcomes and decreased emergency room visits. Smart home technologies and e-health each has unique contributions in the care of older adults, and there is important synergy when the technologies are combined. This will be discussed in a later section of this chapter.
Year 2009 was the first time the International Consumer Electronics Show featured a special section devoted to smart home or high-tech living for seniors. An important example other than motion sensors is a talking pill box that reminds users to take their medicines and which notifies caregivers of omissions (Zagier, 2009). The system utilizes ZigBee wireless technology to receive data from medical sensors. ZigBee consumes low power to transmit data over long periods of time making it suitable for thermometers, blood-pressure monitors, and pulse oximeters. Tele-conferencing between patient and doctor can occur for health status changes detected with the health monitors. Usefulness of these technologies may be self-evident, but there is little research supporting assumptions about effectiveness, and cost-effectiveness. Until there is more research, the role of the technologies and the optimal patient population for the technologies will remain unclearly defined.
Benefits of smart home and healthcare technologies for older adults
In this section, older adults’ perception of SH and healthcare technologies, and the evidence in support of the technologies’ effectiveness is discussed.
Perception of smart home and monitoring technologies
Studies on end users of SH are scarce. Since smart home users are still a small portion of the U.S. population, a survey (Mann at al., 2007) found that 98.2% of 673 respondents were nonusers of the technology. Calling it home automation systems, the study found that 66.6% of 661 respondents were not familiar with the system, 56.3% did not think it would be beneficial to them, and 59.3% were not interested in owning the system even after receiving an explanation. The major reasons for the technologies’ perception as not beneficial were lack of perceived need, high cost, and unfamiliarity. Only 1.8% of the respondents used smart home technology. Among respondents with SH technology, 75% found it very important, and 71.4% were very satisfied. The results indicate that once older adults use SH technology, their perception of its importance and satisfaction will be high.
The researchers of the University of Missouri-Columbia have reported older adults’ perceptions or attitudes toward the technologies. In the aforementioned assisted living place at the TigerPlace II, focus group sessions of 14 older adults (65+) were conducted to find their perceptions of the smart home and healthcare technologies before the installation (Demiris et al., 2008). Overall perceptions of the system applications were mostly useful, but most participants did not agree to the installation of video sensors in their own home because they felt it was unnecessary and an invasion of privacy. Specific responses for each feature were identified. The bed sensors were perceived overall as useful. The gait monitor was perceived as very useful, as most participants expressed concerns about falling and being helpless or not detected in a timely fashion. The video sensor was perceived as beneficial in detecting health emergencies, such as falls. However, even if a video sensor is invisible to participants, they did not want to install it in their own homes. The researchers concluded older adults welcome emergency detection devices, but not home features for prevention through early detection of potential health problems. Participants who had previous experiences with health problems tended to perceive the benefits of these technologies.
Based on their comments, the researchers used monitoring sensors instead of cameras, and followed up with nine residents who lived in the SH. The technology used in the SH consisted of a set of wireless infrared proximity sensors to detect motions. They used lowcost X10 technologies coupled with specialized filtering and analysis. These sensors were installed in existing apartments of older adults who agreed to do so for the purpose of research. They reported the findings from the participatory evaluation of a SH application between Januray 2005 and August 2007 (Demiris et al., 2008). The researchers identified three phases in the process of adoption and acceptance of the technologies: 2-3 weeks for familiarization of technologies, 2-3 weeks for adjustment and curiosity, and full integration as the last phase. In the last phase, residents forgot the existence of the technologies, and the technology did not interfere with daily activities or cause privacy concerns.
In the 29th Annual International Conference of the IEEE, opinions of 30 leaders in the field of aging in the Northeastern United States and Wasthington D.C. were reported (Coughlin et al., 2007). The technologies were considered as having considerable potential to improve one’s safety, but at considerable cost to independence. Constant monitoring as a way to ensure safety and security was regarded as a threat to dignity in one’s own home. Unless individuals are extremely frail and the only other alternative may be nursing home placement, the idea of 24/7 monitoring was not acceptable. Therefore, smart technologies in the home may be a symbol of frailty rather than support for independence and health.
Effectiveness of smart homes
University at Buffalo, New York, using mostly low-cost X10 technologies, retrofitted 50 existing homes of older adults with chronic conditions who lived alone (Tomita et al., 2007). This study was the first randomized controlled trial (RTC) to evaluate the effectiveness of SH use in the United States. Participants selected the smart home technologies to suit their needs in the home. The project did not use continuous monitoring. All smart homes were equipped with window and door security, and an automatic lighting system operated through the participant’s PC where ActiveHome (X10) software was installed. Many participants requested a chime module that was used for an alarm and a medication reminder. The intervention was for two years. At post-test, physical and cognitive functional status of SH users was maintained while those for the control group had significantly declined (p<.05). The difference was apparent in physical dysfunction, instrumental activities of daily living (IADL), mobility, and cognition. At the follow-up, the original 113 participants had reduced to 78. Among the treatment group, 80.4% were living in their own home compared with 65.7% for the control group.
This study also included participants’ two follow-up (1 year and 2 years) perceptions of SH. Overall usefulness was positively perceived by 70.6% at the end of one year and 97.1% at the end of two years. Increased security and safety was the most frequent reason to recommend the technology to other people. This may be the reason for increased mobility. The additional positive impacts were knowledge gain and increased mental health (eg., increased mental stimulus and decreased levels of depression), and increased socialization via the Internet.
SH has limited implementation in the United States with consequent limited evidence of effectiveness. Furthermore, cost effectiveness studies and studies on appropriate technologies for specific populations or groups of older adults are needed.
Internet-based healthcare technology and its’ perception and effects
While smart home technologies tend to focus on the prevention of falls and detection of illnesses based on older adults’ body movements and activities, Internet-based healthcare technology primarily focuses on treating illnesses with prevention of complications as a secondary aim. This technology is variously termed as e-health, Internet-based selfmonitoring system, Internet-based disease management, home health monitoring system, Internet-based telemedicine and telecare, etc.
In the United States, Internet-based disease management grew rapidly in the year 2000 in the healthcare industry. At that time, companies estimated significant cost savings. For example, traditional call-center programs cost $300 to $1,000 per patient per year, while a Web-based program was estimated at about $50 (Managed Care Week, 2000). The Internet continues to be regarded as an excellent compliment to an illness management program. Managed care companies initially pursued disease management for the high-volume chronic diseases diabetes, asthma, and heart disease. A model of disease management from Predictive Services, Inc. utilizes the following process: a virtual counselor guides the participant through an online baseline assessment, who then receives a personalized interactive session weekly. The session is data driven. The patient submits data that is sorted, filtered, and scored to generate personalized responses. This technology has been used by companies for weight management and fitness, pediatric and adult asthma, and women’s and men’s health.
In contrast to studies on SH effectiveness, there are many studies on efficacy or effectiveness of Internet-based healthcare technologies ranging from nonusers’ perceptions of the technology to its effects on symptom management of specific illnesses. However, the vast majority of studies on the effectiveness of these technologies target younger adults. Regarding perception of healthcare technology by older adults, survey results by Mann et al. (2007) found older adults perceived technology as useful for monitoring blood pressure (48.2% of respondents), 21.4% for blood glucose level, 14.4% for weight, 5.2% for heart rate, 2.8% cholesterol level, 2.4% each for mobility problems and falls, and 1.4% each for bladder function and pulmonary problems.
Research on the effectiveness of Internet-based health management shows its success in illness management. A randomized controlled trial was conducted to evaluate the immediate and long-term efficacy of a 12–month web-based intervention for improving diabetes outcomes (Bond, 2005). The study determined intervention effectiveness by measuring physical (glycosylated haemoglobin, weight, and lipid levels), behavioural (monitoring blood glucose levels, feet inspections, diet, and exercise frequency) and psychosocial factors (depression, quality of life, social support, and adjustment to diabetes). The average age of the participants (N=62) was 65.9 years old. All 31 participants in the treatment group were provided with a PC-based computer, a 17 inch monitor, a printer, and dial-up access to the Internet. Intervention participants could access online articles and websites on diabetes and other health related topics, received on-line advice, counselling, and encouragement from a nurse via e-mail, and could participate in weekly nurse-led chat/discussion and a peer support question and answer problem-solving forum. They received instruction regarding the development of personal action plans for diabetes management. These participants were requested to submit vital signs daily (blood sugar levels, medication administration, meal intake, weight and blood pressure). An Internet bulletin board offered the latest news in diabetes management. After five months, 10 of 15 participants decreased their average blood sugar readings by 15 points. All of them increased their exercise duration by 38 minutes on average, and they lost weight of 2.9 pounds on average, decreased in caloric intake by 336 calories, and lowered systolic and diastolic blood pressure by 10 and 5 points, respectively.
Similarly, Internet-based technology was used to promote self-management of patients with heart failure (Tomita et al., 2009). In this pilot study (N=40), all participants were 60 years of age or older. Patients in the treatment group were provided with a PC with Internet and training for computer use. The intervention was intended to empower patients with support from healthcare professionals using the Internet. Self-report of vital signs and targeted exercise on a secure web-site daily made them aware of the causal relationship between health behaviours and symptoms such as body weight and swelling. This RCT identified that after one year, knowledge of heart failure and related healthy behaviour and exercise frequency were increased, illness specific symptoms were improved, and blood pressure and quality of life were improved for the treatment group. Healthcare utilization was decreased for the treatment group. This study attributed the high adherence rate (85%) of the program to a simple web-based recording system, automatic alert for sudden weight gain or loss, patients’ awareness that healthcare providers are watching their records, and healthcare professionals’ personal feedback of the record.
On a very large scale, a one-year RCT was conducted at Stanford University to test efficacy of the use of Internet-based Chronic Disease Self-Management Program (CDSMP) to change health-related behaviours and improving the status of patients with chronic diseases such as heart disease, pulmonary diseases, or type 2 diabetes (Lorig et al., 2006). They tested whether an Internet-based method has the same effectiveness as the original small group method. Comparing 457 patients who used an Internet and e-mail method and a 501 patient usual care control, the study found significant improvements in health status in the treatment, compared with the control group. They concluded that the small-group CDSMP can be carried out by an Internet-based method and it is equally effective (Lorig et al., 2006). A pilot study to compare two methods, Internet/personal digital assistant (PDA) versus face-to-face dyspnea self-management program, for 39 patients with chronic obstructive pulmonary disease (COPD) found that the effectiveness of both methods were similar (Nguyen et al., 2008). In this study, numerous technical challenges occurred with the PDA method and the project had to end earlier than the original plan; it was due to user unfriendliness of the website and PDA application difficulty. In academics as well as in industry, the rapid development of healthcare technologies is recognized; however for older adults, research on effectiveness and cost effectiveness is lacking.
Caregiver perspectives of SH with healthcare technologies
Caregivers for older adults in the United States
In the United States, 44 million individuals serve as informal and unpaid caregivers, and they provide 80% of the care for older adults, (National Alliance for Caregiving & AARP, 2004). Often informal caregivers are in a network including spouses, adult children, extended family, and/or friends. The increase in the number of older adults will hasten the need for informal caregivers due to the growth in the number of elderly individuals living with chronic and disabling conditions (Conway-Guistra, Crowley, & Gorin, 2002). Caregivers provide services ranging from bill payment, transportation, shopping, meal preparation, housework, to personal and complex medical care (Special Committee on Aging, 2001). Informal caregiving can positively impact the physical and mental health of older care recipients, but often at personal costs to the caregivers (Navaie-Waliser et al., 2002). Since caregiving can be stressful for caregivers, the needs of caregivers caring for older adults have been identified: to minimize caregiver burden and depression, and increase positive aspects of caregiving.
Many smart homes with monitoring systems include caregiver components. Healthcare technologies that are less costly and allow for remote caregiving along with safer independence for care recipients can be appealing to consumers. Cook (2007) notes that smart homes can be useful for improving the quality of life of older adults living at home alone in the community, while helping to alleviate the burden associated with caregiving. SH technology allows care recipients to be monitored within their home environment, while caregivers are able to receive health information that can be used to prevent or manage medical conditions. This concept has been implemented in many advanced SH with health monitoring systems.
For older adults living alone without cognitive impairment, personal emergency response systems (PERS) can notify a caregiver or agency that a fall has occurred. When the device is worn on the body, the wearer can press a button in the event of an emergency. Falls are the leading cause of home fatalities in older adults (Fuller, 2000), and a major concern among older adults driving a strong perception of need for these devices. Older adults‘capacity to obtain help in times of distress can reduce worry and stress among caregivers and older adults alike, and may increase caregiver satisfaction. While much research focuses on the negative impacts of caregiving burden, the caregiving process can also include positive aspects. Interventions that promote positive attitudes and perceived satisfaction in the caregiving relationship are important in promoting health and family functioning, and are more likely to be adopted by consumers.
Smart home monitoring interventions and caregivers’ perspectives
While there are a few studies on smart homes and their effects on older adults, only one research study exists regarding SH technology and the caregiver perspective in the United States. A study by Russ (2006) building upon the Smart Home Project by the Technology and Aging Research Project at the University at Buffalo, was conducted with 50 caregivers to older adults with chronic conditions who lived alone. These older adults had previously received computers with Internet capability and training for computer use, along with installation of the smart home (SH) X10 Active Home kit.
The intervention was comprised of installation and training of the X10 Powerhouse personal assistance security console system in the home, along with a wireless call pendant, together known as the PASS. These two devices utilized the telephone line to dial the caregiver for assistance and play back a stored message in the care recipient’s voice. After pressing the call button, the console sounds an alarm to alert the user that the system is activated. The console dials and plays the message three times for the caregiver, and includes a statement asking the caregiver to press 0 on their touch-tone phone. If the listener presses 0, the alarm stops and he or she can listen for 75 seconds, at which time the care recipient can speak their message asking for help. If the phone has not been answered or an answering machine comes on, the console will dial the next of up to four stored telephone numbers. Seventyfive seconds after pressing 0, the alarm resumes and stops after four minutes unless the care recipient presses the STOP button on the call pendant, which will stop the alarm and reset the console. This stand-alone device was chosen because of its low cost and the relative ease of installation and use. The PASS had a onetime cost of $50.00 and no service or monitoring fees; more attainable for many people. Installation and initial training were provided. Ongoing technical support was provided, when necessary. A friend or family member was identified as the informal caregiver of interest for this study.
Caregivers were assessed for burden, depression, and caregiving satisfaction. The study compared the PASS users (treatment) and non-PASS users (control) who were further divided into e-mail users and non-users. The result showed that the PASS was effective in preventing an increase in caregiver depression and burden, but did not have any effect on caregiving satisfaction. E-mail use was found to be effective in preventing a significant increase in caregiver depression and burden in specific segments of the sample, but again had no effect on caregiving satisfaction. PASS and e-mail use combined was the most effective method to prevent increases in caregiver depression and burden over one year, while enhancing the relationship with the care recipient.
The primary concerns of the caregivers, for both the treatment and control groups (over 93% in both groups), were falls or injury as opposed to home security (less than 7%). Onehundred percent of the caregivers in the treatment group reported that they were pleased that their care recipients had the smart home, including the PASS, because of decreased worry about the care recipient’s safety as a consequence of living alone.
PASS does not require the cost-prohibitive monthly monitoring fees seen with commercial personal emergency response systems. Cost is an important consideration, since over onehalf of the care recipients had an annual income of less than $20,000. Older adults with disabilities and annual household incomes less than $20,000 were more likely to report inadequate assistance with activities of daily living and unmet needs. This puts these older adults at increased risk for adverse health outcomes and increased likelihood of institutionalization (Desai et al., 2001). The combined paid and unpaid costs to families for community care of frail older relatives ranges from $10,000 to $20,000 annually, depending upon their condition. These out-of-pocket costs may make formal care prohibitive (Allen, Foster, & Berg, 2001). Thus, the PASS is a feasible, low cost resource for these individuals. This technology is an option that can contribute to making the home a safe alternative to long-term care for many older adults.
A study from outside the United States was included here because of the paucity of data from the United States. Rialle et al. (2008) surveyed 270 families in France caring for persons with Alzheimer’s disease and other dementia on their perceptions related to new smart home technologies to aid in dementia care at home. Two distinct groups were identified among family caregivers: one in favor of the use of technology, and those not in favors. Female caregivers were more willing to consider these technologies as an aid to caregiving. Although this result may be cultural, the study emphasizes the need to carefully consider the demographic characteristics of the caregiver in the development and targeting of healthcare technologies for use with older adults.
Increasingly, the perspective and the needs of caregivers are considered in the development of smart homes for older adults. This technology can potentially reduce caregiver depression and burden, and enhance the relationship with the care recipient. However, the benefits of smart homes may not be universal for all users, and are not fully understood.
The role of SH with healthcare technology and a conceptual framework
Technology that is needed
Physical and cognitive function is major determinants of an older adult’s ability to live independently. The combination of the physiology of aging and chronic disease makes the maintenance of function a challenge with advancing age. The major illnesses affecting older adults’ lives include arthritis, cardiovascular health, cancer, diabetes, epilepsy, obesity, oral health (Centers for Disease Control and Prevention, 2008). A healthy diet, smoking cessation, and exercise are important lifestyle elements that are part of disease management for many of the major chronic diseases. Promoting healthy behaviours should be a significant element of SH with healthcare technology.
Telehealth and e-health technologies specifically focus on monitoring vital signs for managing a chronic illness by healthcare professionals. Based on limited studies, older adults with chronic conditions accept monitoring for chronic conditions as opposed to lifestyle monitoring. In fact, the awareness that a health care professional is paying attention to the records is one of the reasons for high adherence to a health regimen. Even so, cost limits extensive implementation of the technology. What is lacking in SH with healthcare technology is inexpensive and secure technology that helps community-dwelling older adults with chronic conditions (1) manage their illnesses with monitoring by a healthcare professional and/or caregivers, and (2) maintain their physical and cognitive function without being monitored but connected to healthcare providers and caregivers. In addition, one of the most essential factors of the technology is that it should be incorporated into existing homes, so that older adults do not have to move to a new facility.
These technologies can be used for home therapy after surgery, but also need to be used after nurses’ home visits end. The hospital stay time is becoming shorter due to changes in health insurance coverage policy. To prevent another hospitalization and emergency visits, and eventual nursing home placement, these technologies should be utilized daily for maintaining health, functional status, and quality of life or even improvement in older adults with various levels of conditions. It appears insufficient efforts have been made to provide these technologies for less frail older adults who do not require constant monitoring. The following section discusses the technology necessary to address needs of less frail older adults.
SH with healthcare technology
Although the optimal patient group has yet to be defined, one clear role for SH with healthcare technology is to enhance safety and promote physical and cognitive activities. The monitoring system should be developed with the user in mind. The system needs to be able to alert the user, as well as caregivers and first responders, when necessary.
Falls and safety prevention and detection: Sensors can detect when there is no movement or movement in an unusual location and issue a warning in an appropriate sequence. Or, a user may activate a personal alert.
Safety and security monitoring: It includes automatic control of water temperature, ambient temperature, stove and oven shut-off, lighting, window and door security, intruder alarm, and visitor identification. The frequency of a refrigerator door movement also can be recorded. Older adults may control timing and intervals of these devices through operation of a computer.
Health status monitoring: It can be also done by the SH such as under-the-bed sensors for detecting sleep patterns, a medication reminder, an appointment reminder, a toilet bowl sensor to check frequency of its use and health data such as the sugar level in urine. They may also include checking and recoding of vital signs such as blood pressure, glucose level, body temperature, pulse, weight, cholesterol, medication adherence, and interactions. A significant change in pattern or a significant delay in readings each serves as a trigger for an alert. Automatic transfer of vital signs has a purpose, but users benefit from knowing about and following the data. Audible and visual feedback from the measuring device can be very helpful when the user is monitoring his or her health status.
Nutrition/diet: One’s caloric intake can be monitored and an audible and visual reminder alerts the person of a recommended consumption level.
Memory aids: They include reminder system announcing upcoming appointments or events and medication are useful for any older adult.
Physical activity level: This can be monitored without a video camera. This includes the amount of movements including exercise, ADL, IADL, and leisure. A wearable device informs about an exercise level and warns if there is evidence of excessive exercise. Video conference technology can promote a group exercise program and allow instructors to model the exercise. Group exercise and instruction may be particularly valuable during inclement weather.
The main concerns for these technologies are cyber security, privacy issues, costs, lack of human responders, and user friendliness combined with training.
Cyber security issues: SH with monitoring system is open to security vulnerabilities due to the network interconnection of different monitoring systems and SH terminals. Confidentiality, integrity, and availability have to be considered. Efficient encryption solution is essential.
Privacy issues: Strict control on the use and access to the monitoring data is an essential privacy standard. Older adults may become more involved if they control most of the monitoring data. The monitoring can give the older adult point-of-care feedback about their daily health status and prompt access to a health professional if that is warranted.
Costs: When the reporting goes directly to the user, the costs are much lower than when external entities participate in continuous monitoring.
Lack of human responders: The absence of a routine external monitor may leave users with the perception that there is no human invested in the process. Prompt response to alerts can allay some of those fears.
User friendliness: Older adults need simpler and less complicated interface and operation; training is another important element.
In summary, the role of SH with healthcare technology is to empower older adults to take care of their health and function themselves in their own homes. Most importantly, these technologies should promote healthy behaviours by raising awareness in older adults about the causal relationship between their daily activities and health and functional status. Figure 1 summarizes responsible parties for monitoring at the continuum of older adults’ physical and cognitive function and their health status. Healthy older adults primarily doing selfmonitoring is illustrated in the upper left in the diagram. The diagram illustrates a gradual decline in function moving clockwise. Ultimately, health monitoring may become the exclusive responsibility of professional caregivers for some older adults.
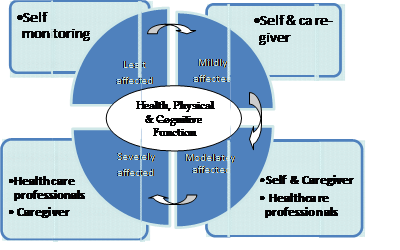
Fig. 1. Responsible parties for older adults’ activity monitoring in relation to their health and physical and cognitive function
Model toward Optimal Management for Independence through Technological Adoption
A Model toward Optimal Management for Independence through Technological Adoption (M-TOMITA) had been proposed by the two authors in this chapter to identify the effectiveness of e-health for older adults with heart failure (Tomita et al., 2009). The model is an application of the original social support theory, to human support through technology utilization. It illustrates the role of e-health as a means to provide four types of support: informational, instrumental, emotional, and appraisal. The purpose of the support is to assist an individual to advance five stages of health behaviours in Transtheoretical model (TTM): precontemplation, contemplation, preparation, action, and maintenance to manage their illness or health. The advantage of use of technology is to give users power to use services and information provided through technology at any time and any place. Also it gives users confidence that they can use advanced technology, can manage their health, and can connect to healthcare professionals instantly. This concept is based on mass media’s Uses and Gratification theory.
These same concepts can be applied for SH with healthcare technologies. In this case, the purpose is not only to manage chronic illnesses, but also to maintain and improve functional status. SH should provide older adults feedback about health patterns and functional status which will lead to increased understanding of behaviour. This is informational support. SH should allow their review of records or input about activities and health. The involvement in this process is important so there is awareness of health/function behaviour, but also an understanding of cause and effect between behaviour and health/function. Instrumental support provides automatic alerts to the user, caregivers, healthcare providers and first responders. SH technologies provide appraisal support by evaluating one’s behaviour, but if an automatic feedback is programmed, emotional support may also be provided by caregivers, and healthcare professionals provide emotional support. This process is continuous through SH with healthcare technologies.
The difference between the model’s application to e-health and SH with health technology is that the latter may not be helpful to advance older adults stages of health behaviours from precontemplation, contemplation, to action. But the technology may be effective in advancing the stage from action to maintenance stage. Another advantage of this type of technology is that it is easy to make all readings and records available to caregivers. Even if an older adult is not motivated to self-manage/monitor behaviours, there is an opportunity for caregivers to assist with the monitoring. For willing caregivers, the technology may reduce adverse psychological effects of caring for older adults. The model is summarized in Figure 2.
Conclusion
Although the constant external monitoring (by others) feature of SH is useful for frail elders in assisted living facilities and nursing homes, it is not likely to be accepted by, and available for the majority of older adults who live in their own homes. Inexpensive SH technologies that can be used for the purpose of self-monitoring of safety, health, and functional status in existing homes are urgently required. The role of these technologies is to empower older adults for self-management for independent living and to minimize adverse effects on their caregivers’ stress. The built-in warning system based on readings/reports collected by SH with healthcare technologies should send automatic alarms to self, caregivers, healthcare providers, and/or a fire department. The possibility of these SH with healthcare technologies is bountiful, but the research on its effectiveness and cost-effectiveness should be conducted concurrently, as they develop.
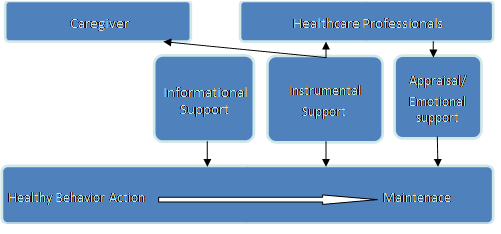
Fig. 2. Model toward Optimal Management for Independence through Technological Adoption applied for smart home with healthcare technologies


